Fibroblasts involved in healing spur tumor growth in cancer
Vital to healing wounds, fibroblasts have a "misguided" response to cancer cells, according to TAU researchers
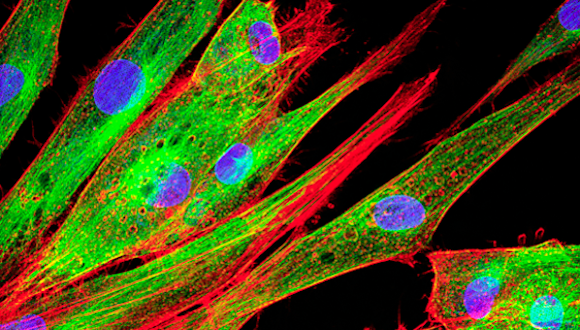
Support this researchThe connective tissue cells known as fibroblasts are vitally important for our recovery from injury. Sensing tissue damage, they gravitate to the site of a wound, instigating an inflammatory response that mends damaged tissue.
A new Tel Aviv University study published in Nature Communications on September 26 finds that fibroblasts also play a devastating role in the development of breast cancer. In cancer tumors, fibroblasts are triggered to respond to tissue damaged by tumors and create inflammation. This inflammation facilitates tumor growth as well as metastases in the lungs.
“We have shown, for the first time, that in breast cancer these fibroblasts activate a ‘misguided’ wound healing response, responding to the tissue damage caused by the cancerous growth,” explains Prof. Neta Erez of TAU’s Sackler Faculty of Medicine, who led the research for the study. “Inhibiting these inflammatory signaling pathways may be beneficial in preventing metastatic relapse of breast cancer.”
The study was conducted by former TAU student Yoray Sharon and TAU MD-PhD student Nour Ershaid in Prof. Erez’s lab at TAU’s Department of Pathology.
According to the study, the inflammatory response of fibroblasts not only supports local tumor growth in the breast, but it also creates a hospitable niche for metastatic growth in the lungs. “The fibroblasts are ‘activated’ and, because of this activation, they recruit immune cells and affect blood vessels,” adds Prof. Erez. “In other words, breast tumors ‘hijack’ the physiologic response to tissue damage to facilitate their growth, and create a niche in a distant organ, the lungs, by ‘remote control.'”
Research for the study was performed using transgenic and transplantable mouse models of breast cancer, and validated in human samples of breast cancer and in human expression data.
The researchers isolated fibroblasts in transgenic mice from different stages of breast carcinogenesis and profiled the expression of all their genes. They were then able to identify that the inflammation pathway is unregulated in cancer-associated fibroblasts, as compared with fibroblasts isolated from normal mammary glands. Finally, they performed functional experiments to understand the role of this pathway in breast cancer.
“Our findings encourage the design of preclinical and clinical studies to examine the benefits of targeting the inflammation pathway in breast cancer, which may be effective in blocking metastatic relapse,” concludes Prof. Erez. “We are now studying the microenvironment of metastasis in an effort to identify targets for preventive intervention that may inhibit metastatic relapse.”