TAU research develops technique to inhibit skin cancer metastasis to the brain
New approach inhibited spread of cancer by 80%
Support this researchResearchers from Tel Aviv University (TAU) have deciphered a mechanism that enables skin cancer to metastasize to the brain and managed to delay the spread of the disease by 60% to 80% using existing treatments.
The study was led by Professor Ronit Satchi-Fainaro and PhD student Sabina Pozzi of TAU’s Sackler Faculty of Medicine. The results were published in the scientific journal JCI Insight.
“In an advanced stage, 90% of melanoma (skin cancer) patients will develop brain metastases,” explains Professor Satchi-Fainaro. “This is a puzzling statistic. We expect to see metastases in the lungs and liver, but the brain is supposed to be a protected organ. The blood-brain barrier keeps harmful substances from entering the brain, and here it supposedly doesn’t do the job — cancer cells from the skin circulate in the blood and manage to reach the brain. We asked ourselves with ‘whom’ the cancer cells ‘talk’ to in the brain to infiltrate it.”
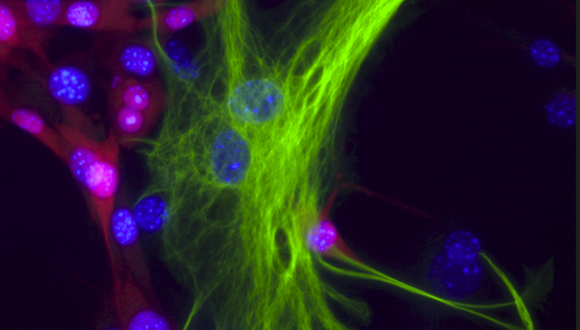
The researchers found that, in melanoma patients with brain metastases, the cancer cells “recruit” cells called astrocytes, star-shaped cells found in the spinal cord and brain which are responsible for homeostasis, or maintaining stable conditions, in the brain.
“The astrocytes are the first to come to correct the situation in the event of a stroke or trauma, for example,” says Professor Satchi-Fainaro. “It is with them that the cancer cells interact, exchanging molecules and corrupting them. Moreover, the cancer cells recruit the astrocytes so that they do not inhibit the spread of the metastases. As such, they create local inflammation in the melanoma cells-astrocytes interaction areas that increase the permeability through the blood-brain barrier, as well as the division and migration of the cancer cells.
“The communication between them is reflected in the fact that the astrocytes begin to secrete a protein that promotes inflammation called MCP-1, also known as CCL2. In response to this, the cancer cells begin to express its receptors CCR2 and CCR4, which we suspected to be responsible for the destructive communication with the astrocytes.”
To test their hypothesis, Professor Satchi-Fainaro and her team tried to inhibit the expression of the protein and its receptors in genetically-engineered lab models and in 3D models of primary melanoma and brain metastases. They used both an antibody (biological molecule) and a small molecule (synthetic), designed to block the MCP-1 protein. They also employed CRISPR technology to genetically edit the cancer cells and cut out CCR2 and CCR4, the two genes that express the two relevant receptors. With each of the methods, the researchers were able to delay the spread of metastases.
“These treatments succeeded in delaying the penetration of the cancer cells into the brain and their subsequent spread throughout the brain,” says Professor Satchi-Fainaro. “It’s important to note that melanoma metastases in the brain are very aggressive with a poor prognosis of 15 months following surgery, radiation, and chemotherapy. We reached a 60% to 80% delay, depending on the stage of the intervention. We achieved the best results with the treatment conducted immediately after surgery to remove the primary melanoma, and we were able to prevent the metastases from penetrating the brain.
“I believe that the treatment is suitable for the clinic as a preventive measure,” Professor Satchi-Fainaro concludes. “Both the antibody and the small molecule we used — which are primarily intended to treat sclerosis, diabetes, liver fibrosis, and cardiovascular diseases, as well as serve as a biomarker for other types of cancer — have already been tested on humans as part of clinical trials. Therefore, these treatments are considered safe, and we can try to repurpose them for melanoma.”
The research was conducted in collaboration with additional TAU scientists and physicians, including Professor Adi Barzel, Dr. Asaf Madi, Professor Iris Barshack, Professor Eran Perlson, and Professor Inna Slutsky. International researchers also participated in the study, including Professor Eytan Ruppin from the US National Institutes of Health (NIH), Professors Henry Brem and Thomas Hyde from Johns Hopkins University, and Professor Helena Florindo from the University of Lisbon.
The study was funded by the European Research Council (ERC), the Melanoma Research Alliance (MRA), the Kahn Foundation, the Israel Cancer Research Fund (ICRF), and the Israel Science Foundation (ISF).